Health Subrogation
Streamline your claim recovery process to put more money back into your Medicaid program.
Let’s talk health subrogation.
We understand that the reimbursement process in Medicaid third party liability (TPL) can be complex. At KL&A, health subrogation is a large part of our comprehensive third party liability offerings, so we know all the ins and outs of the many processes involved. Our team of experts has years of experience in health subrogation for Medicaid programs – in both software development and navigating the landscape of subrogation to ensure that you recover the maximum amount possible.
We offer a range of software solution features tailored to the claim process that can be accompanied by our services to perform the work on your behalf – or set your staff up for success. So if you’re looking for a reliable and experienced partner to help you tackle health subrogation, look no further than our company.
Take what you want, build what you need.
Whether you’re looking for software that will help you do the work yourself, in need of KL&A’s services along with the technology, or require a modular mix and match approach of solutions and services, we offer it all. By leveraging our existing Medicaid third party liability technologies, we can create a customized approach for your organization based on the features you need. Let us help you get more returns and maximize your reimbursement so that you can help more people get the care they need.
Claim Identification & Billing Support
Streamline your claim recovery process with the option to request additional customizations for all your unique billing preferences and needs.
- Efficiently identify and track claims that may be eligible for third-party reimbursement.
- Improve billing efficiency and third party providers’ compliance with Medicaid regulations.
- Lighten the daily workload by automatically identifying claims and generating invoices.
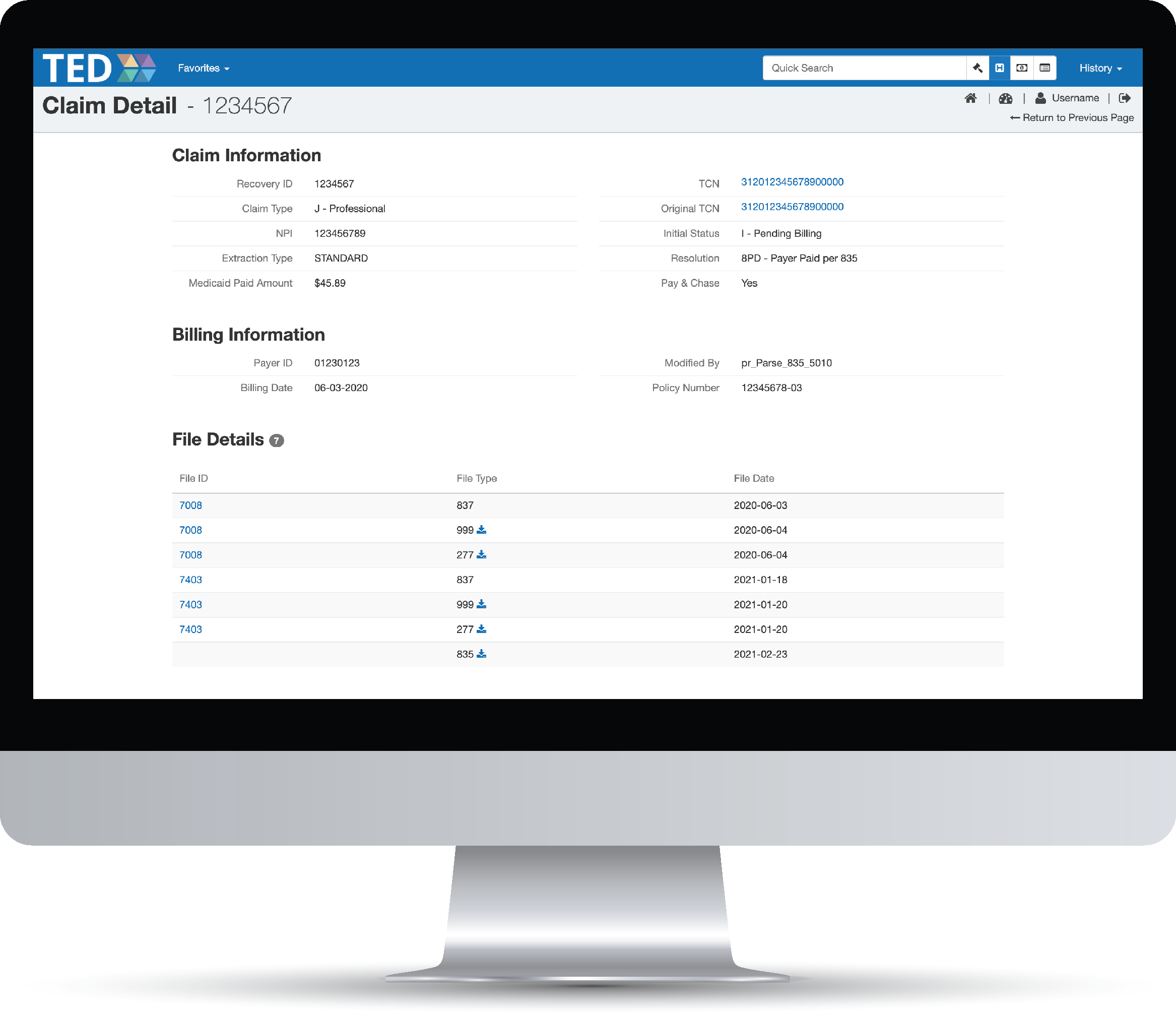
Claim Identification & Billing Support
Streamline your claim recovery process with the option to request additional customizations for all your unique billing preferences and needs.
- Efficiently identify and track claims that may be eligible for third-party reimbursement.
- Improve billing efficiency and third party providers’ compliance with Medicaid regulations.
- Lighten the daily workload by automatically identifying claims and generating invoices.
Payer Onboarding Support For Subrogation Billing
Provide flexibility and simple onboarding for new payers through generating and processing HIPAA compliant electronic data interchange (EDI) transactions such as X12 and NCPDP.
- Tailor the system to your needs with customizable configurations for different insurance companies.
- Easily set up connections with payers or their clearing houses to process your claims. Our experts’ familiarity working with a wide variety of payers makes configuration a breeze.
- Simplify Medicaid subrogation billing with tailored validation rules and compliance status tracking.
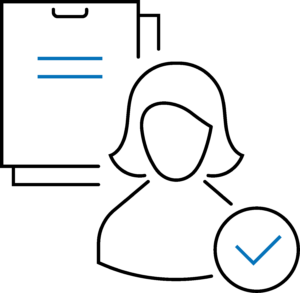
Payer Rejection Monitoring & Auditing
Improve response processes with automatic tools to help handle rejections and rebilling of claims. Never miss a thing with increased staff oversight providing the ability to review rejections that can not be corrected automatically.
- Easily follow the claim lifecycle to determine improper rejections due to Medicaid-specific requirements, increasing the potential number of recoveries made despite an initial rejection.
- Generate reports and alerts to quickly identify payer rejections and analyze the underlying causes.
- Ensure third-party payer responsibility for liable payments by effectively tracking and analyzing each payer rejection to address issues that prevent reimbursement.
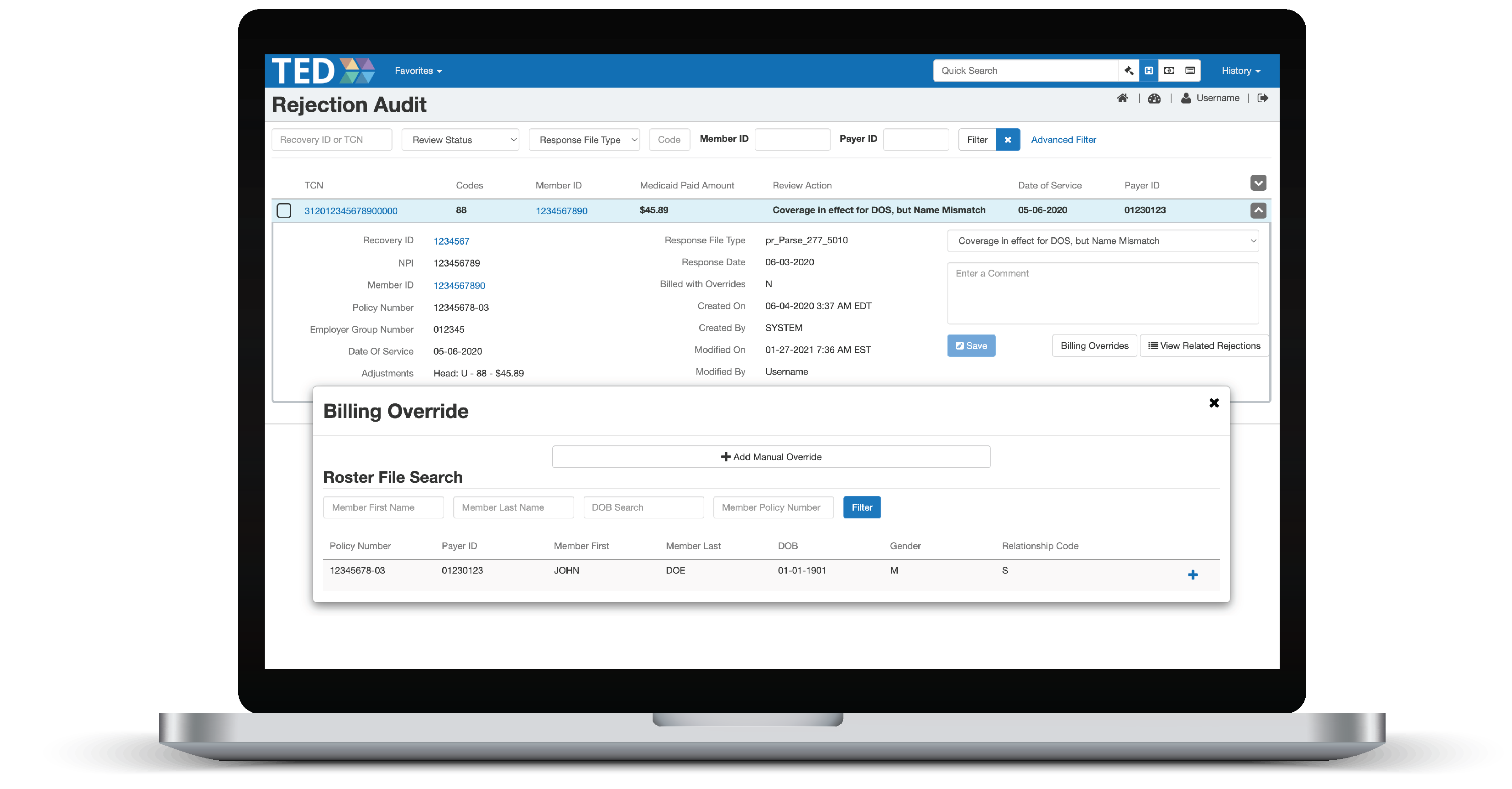
Payer Rejection Monitoring & Auditing
Improve rejection processes with automatic tools to help handle rejections and rebilling of claims. Never miss a thing with increased staff oversight providing the ability to review rejections that can not be corrected automatically.
- Easily follow the claim lifecycle to determine improper rejections due to Medicaid-specific requirements, increasing the potential number of recoveries made despite an initial rejection.
- Generate reports and alerts to quickly identify payer rejections and analyze the underlying causes.
- Ensure third-party payer responsibility for liable payments by effectively tracking and analyzing each payer rejection to address issues that prevent reimbursement.
Claim Accounting Reconciliation
of Payer Remittances
Put more money back into Medicaid by easily identifying missing or incorrect payments through reconciling checks received from payers with the EDI response files.
- Stay informed and ease your worries with full-circle tracking of the repayment process.
- Lighten the administrative burden on both your staff and payers by simplifying the remittance process and reducing the need for manual paperwork.
- Ensure timely and accurate payment reconciliation with a centralized platform for tracking payments.
Oversight Tools
Understand what’s going on beyond just the numbers by easily identifying issues and gaining new insights with our user-friendly graphs and reports to monitor the automated billing and response process.
- Keep TPL leadership, your team, and vendors informed by visually communicating key information that can be used to troubleshoot or inform data-driven decision-making.
- Proactively identify patterns and issues with access to real-time data.
- Optimize your auditing process with this end-to-end billing process oversight dashboard.
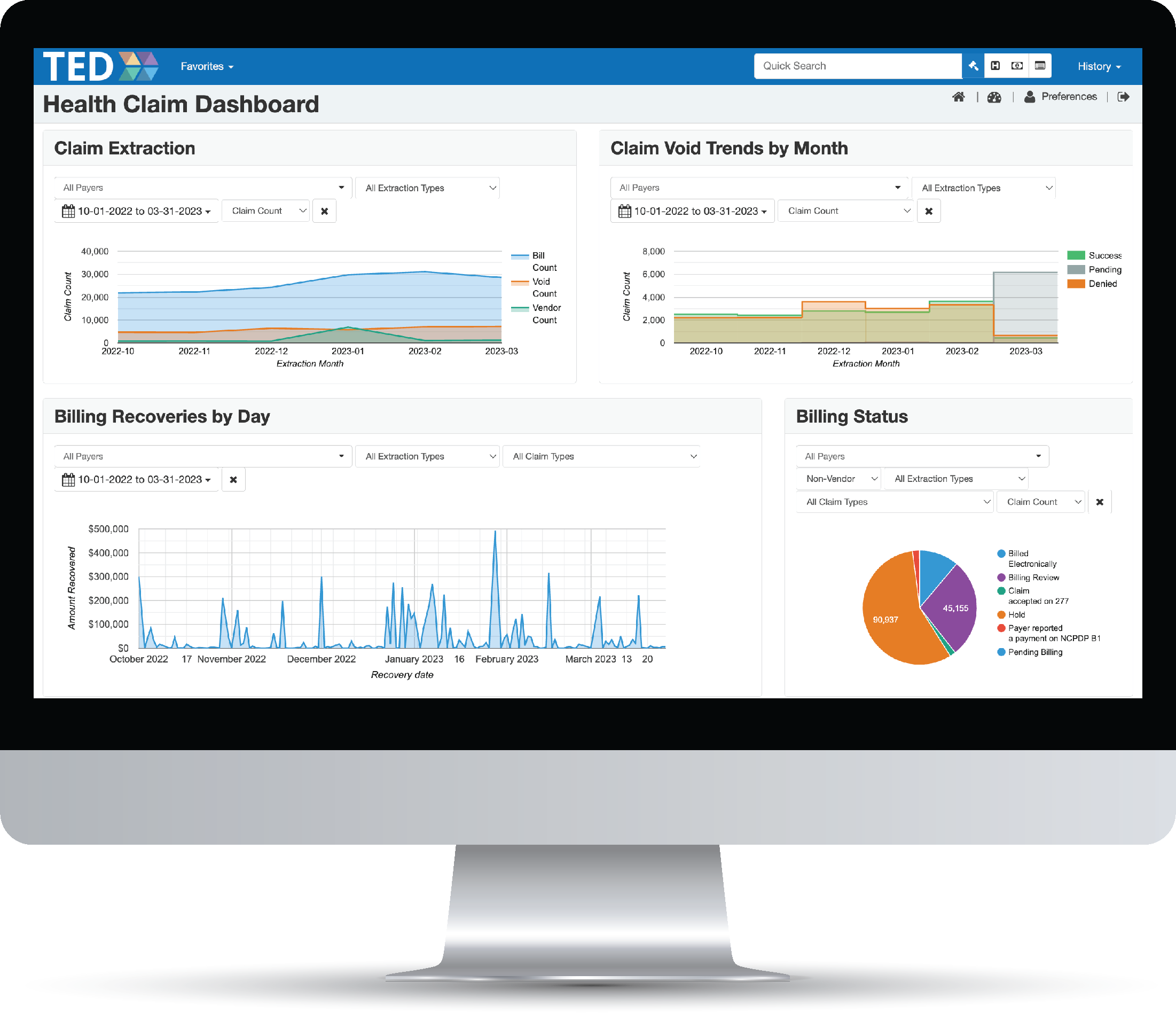
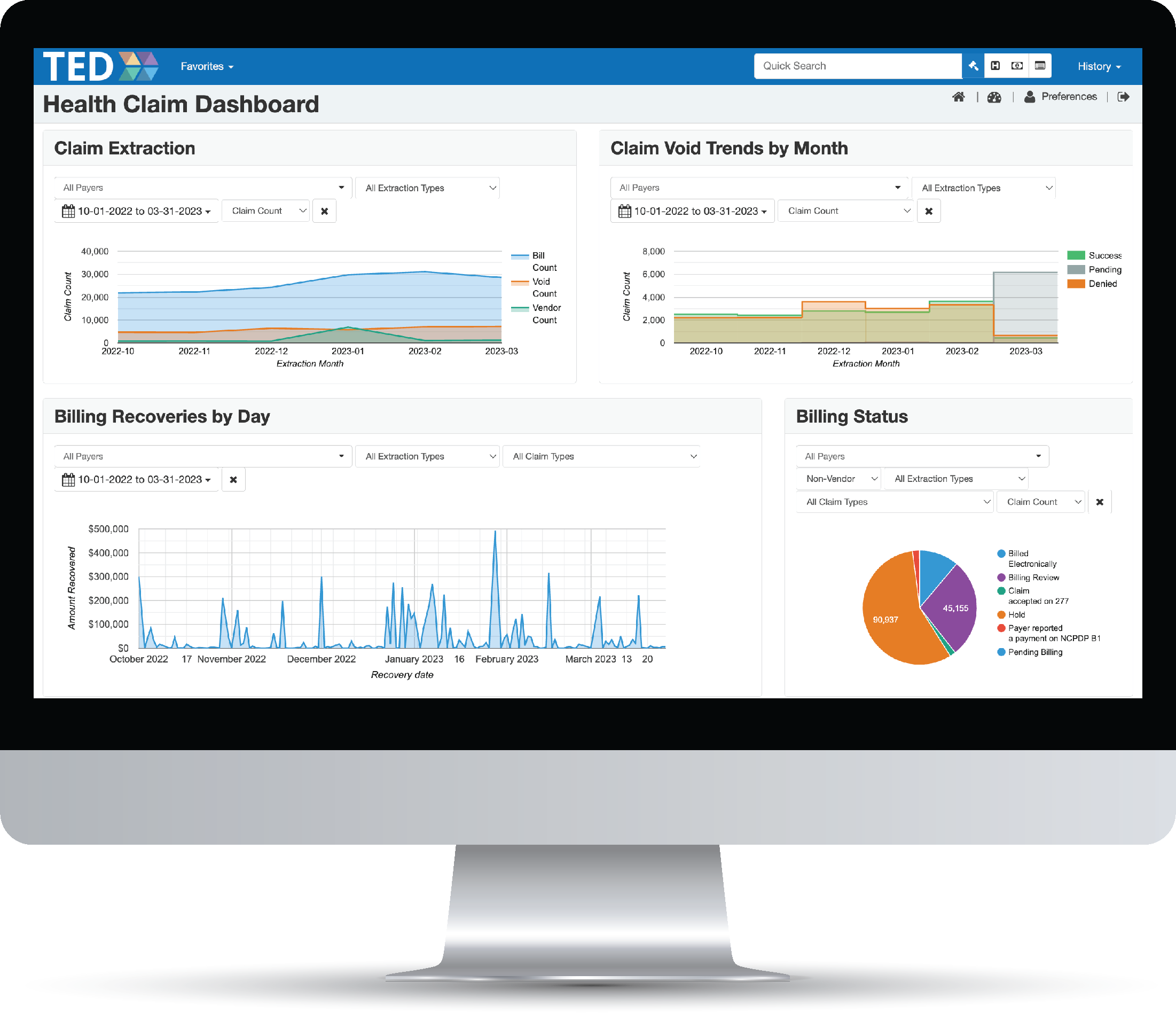
Oversight Tools
Understand what’s going on beyond just the numbers by easily identifying issues and gaining new insights with our user-friendly graphs and reports to monitor the automated billing and response process.
- Keep TPL leadership, your team, and vendors informed by visually communicating key information that can be used to troubleshoot or inform data-driven decision-making.
- Proactively identify patterns and issues with access to real-time data.
- Optimize your auditing process with this end-to-end billing process oversight dashboard.
Here’s the short version of it all.
You name it, we create it. And with our team of experts on your side, we can provide valuable insights into the claim process through your newly modernized system to help you make informed decisions and maximize your returns. When it comes to health subrogation, we excel as a solution provider and a service.
Optimize The Process
Our user-friendly solutions provide streamlined workflows, and automated processes to assist with follow-up on billing information conflicts to help save you time.

Integrate With Ease
Overloaded with too many systems? We won’t add to the pile. We design to easily integrate with other systems allowing for staff to stay in one system instead of checking multiple.
Maximize Your Everything
More time saved and money recovered. No matter the size of your TPL division you can effectively leverage a small or large amount of staff. Our solutions will allow you to work smarter, not harder to accomplish even more work.
Evolve With Changes
There’s no one-size-fits-all solution. Whether you find yourself faced with shifting working environments, policy changes, or newly desired configurations, our solutions are built to adapt. We design for the current state of work with secure remote access and can tailor a system to meet your unique needs
But wait, there’s more!
Looking to couple your health subrogation efforts with another TPL area? Our comprehensive third party liability services are modularly designed for you to choose what you need, how you need it.

INSURANCE COVERAGE
The best way to maximize your post payment recoveries is to have the most accurate and up to date coverage. Our tools can help you identify coverage before payment to help with cost avoidance.

VENDOR OVERSIGHT
Whether you’re outsourcing the work, operating fully in house, or a mix of both, stay informed with our suite of tools, including detailed dashboards and reports.
Caught in a never-ending billing nightmare?
Let us help you wake up! Our team is here to navigate the confusing world of Medicaid health subrogation and ensure you get maximum claim recoveries.